Did you know that about one-third of adults report having trouble sleeping? Interestingly, between 4 to 22% of them meet the criteria for an actual insomnia disorder. This shows a major concern among Americans. With over 50 million Americans battling chronic sleep issues, knowing how to diagnose insomnia is key. Being able to accurately identify this sleep disorder is critical. Because, apart from messing with sleep, it can also lead to serious mental health issues. The process of diagnosing sleep disorders includes knowing the symptoms and using tools from the DSM-5. This article will explore the complex world of insomnia. It aims to give you important information on how it is diagnosed.
Key Takeaways
- About one-third of adults report insomnia symptoms.
- 4 to 22% of those adults meet the criteria for insomnia disorder.
- Clear diagnostic criteria are essential for effective treatment.
- Insomnia is linked to other mental health disorders in about 40-50% of cases.
- More than 50 million Americans suffer from chronic sleep disorders.
- Understanding the DSM-5 criteria is crucial for proper sleep disorder diagnosis.
Understanding Insomnia and Its Impact
Insomnia is a big problem for public health. It’s more than just trouble sleeping. It affects a person’s overall health. To really understand insomnia, we need to look at how common it is and who gets it. This helps health experts make the right diagnosis.
Definition of Insomnia
The DSM-5 sees insomnia as a disorder where people are unhappy with their sleep. Insomnia can show itself in different ways, such as:
- Difficulty initiating sleep
- Difficulty maintaining sleep
- Early morning awakening with an inability to return to sleep
To be diagnosed, you must have these issues for at least three nights a week. You must also have enough chance to sleep well. Insomnia must not be because of other disorders or caused by medicine or health issues.
Prevalence and Who It Affects
Research shows about 30% of adults worldwide report symptoms of insomnia. If we also consider daytime problems, this number falls to 10%. Insomnia is more common in women and the elderly. Other factors, like having certain diseases or mental health issues, can increase the risk. Many with insomnia also deal with conditions like depression or anxiety.
About 40% of people with insomnia have a psychiatric condition. This shows how crucial proper diagnosis and treatment are. Insomnia not only harms health but also leads to higher medical costs and a greater risk of accidents. Understanding all aspects of insomnia is key to tackling this issue.
Common Symptoms of Insomnia
Insomnia has many symptoms that can disrupt daily life. It’s key to recognize these to find the right treatment. This matches the guidelines for evaluating insomnia.
Difficulty Falling Asleep
Falling asleep can be hard for many. Some lie in bed for 20 to 30 minutes, trying to sleep. This can make them anxious about sleeping.
Challenges in Maintaining Sleep
Staying asleep is tough for those with insomnia. They often wake up several times at night. This leads to feeling tired and grumpy the next day.
Early Morning Waking
Waking up early and not being able to go back to sleep is common. This leaves people feeling tired all day. It’s important to keep track of these signs.
Knowing about these symptoms helps diagnose insomnia. If they impact your life or mood, get help. You might need to talk about your health history or do a sleep study. Learn more about treating sleep problems at insomnia evaluation guidelines.
Diagnostic Criteria for Insomnia
Chronic insomnia disorder is defined using criteria from the DSM-5. These guidelines state that one must experience sleep problems at least three nights a week. These issues must last for over three months. Also, these sleeping problems must cause significant distress or problems during the day to be considered insomnia.
Overview of DSM-5 Criteria
The DSM-5 criteria for insomnia focus on ruling out other reasons for sleep problems. To diagnose insomnia, the following must be true:
- Sleep complaints occurring at least three times weekly.
- Symptoms persisting for at least three months.
- Exclusion of other sleep disorders, medical conditions, mental disorders, or substance use.
Differences from DSM-IV Criteria
The DSM-5 now uses a stricter method to understand insomnia compared to the DSM-IV. Earlier, even unrefreshing sleep could be considered a symptom. This change shows a deeper understanding of how complex and impactful chronic insomnia is.
Now, insomnia is classified more clearly, separating chronic insomnia from other sleep problems. This clarity helps in choosing the right treatment. It addresses the significant effects of insomnia on health, well-being, and finances, with insomnia costing the US between $12 to $14 billion yearly.
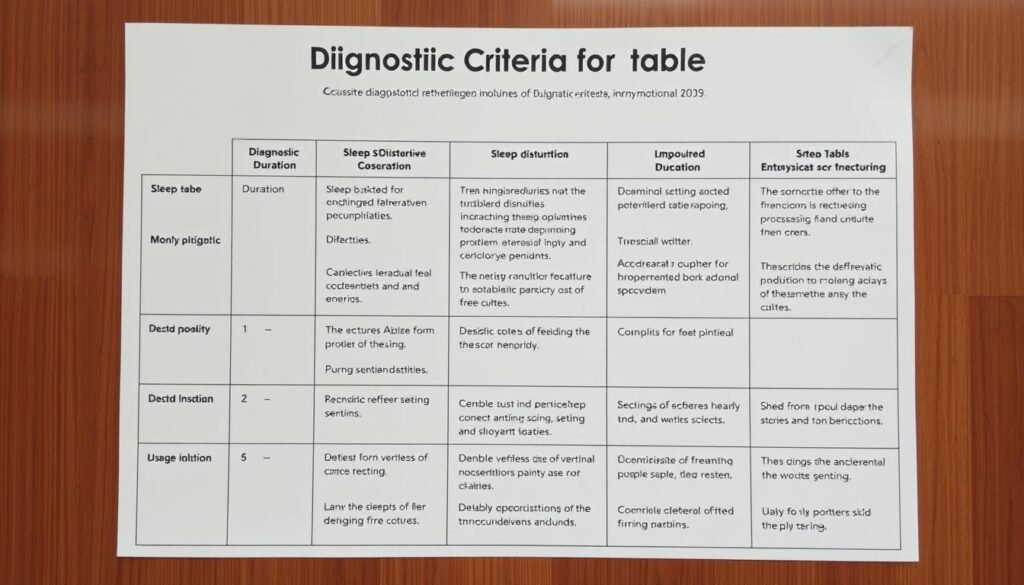
| Criterion | DSM-IV | DSM-5 |
|---|---|---|
| Frequency of Symptoms | Variable | At least 3 times a week |
| Duration of Symptoms | Variable | At least 3 months |
| Exclusion of Other Conditions | Less emphasis | Strong emphasis on exclusion |
| Daytime Impairment | Not always specified | Must cause distress or impairment |
These changes in diagnosis help pinpoint chronic insomnia more accurately, leading to better treatment. For more info, check relevant literature. This knowledge aids doctors and helps patients understand their insomnia better.
Sleep Disorders and Insomnia Diagnosis
Getting the right diagnosis for insomnia is key. It can be mixed up with other sleep issues. To tell insomnia apart from conditions like sleep apnea and restless legs syndrome, doctors carefully look at symptoms. Knowing the difference helps in picking the right treatment.
Distinguishing Insomnia from Other Sleep Disorders
It’s easy to confuse insomnia with other sleep issues. An accurate diagnosis of insomnia is crucial. While insomnia makes it hard to fall or stay asleep, other conditions have their own signs:
- Sleep Apnea: This causes breaks in breathing during sleep, leading to tiredness in the day.
- Restless Legs Syndrome: It’s when there’s a strong need to move the legs while resting.
- Parasomnias: These are unusual actions during sleep, like sleepwalking or having night terrors.
Identifying the specific symptoms of these disorders helps in treating insomnia correctly.
The Role of Comorbid Conditions
Many with insomnia also have conditions like anxiety or depression. This makes diagnosing insomnia more complex. The overlapping symptoms can hide the real sleep problems. Some facts include:
- Chronic insomnia happens at least three times a week for more than three months.
- Women are more likely to suffer from insomnia.
- Age, lifestyle, stress, and family history can influence insomnia.
Doctors need to look at all these aspects to better treat insomnia. A full look at everything allows for customized treatment plans. This approach tackles both insomnia and its related issues.
Insomnia Evaluation Guidelines
Understanding insomnia starts with knowing the patient’s situation. A good initial check-up includes a deep interview. This covers life habits, health history, and sleep routines. These help find the reasons behind insomnia. By having this full picture, experts can follow the right steps for diagnosing.
Initial Assessment and Clinical Interview
The interview looks at many parts of the patient’s life. It focuses on:
- Sleep patterns: Checking how much and how well the patient sleeps.
- Healthcare background: Looking into health issues that affect sleep.
- Daily routines: Talking about activities that might impact how well someone sleeps, like drinking caffeine or using screens before bedtime.
This complete check-up is key for understanding what’s wrong. A lot of patients mention issues tied to chronic insomnia. These cases need more checking.
Utilizing Sleep Diaries for Assessment
A sleep diary is very helpful for figuring out insomnia. Patients write down their sleep details, including:
- When they go to bed and get up.
- How often they wake up at night.
- How they feel about their sleep quality and length.
Diary entries show sleep patterns and issues that are hard to spot otherwise. A detailed sleep diary makes patient-doctor talks more fruitful. This helps in making a plan that really suits the patient. For tips on discussing insomnia and treatments with your doctor, check out this resource.
Insomnia Screening Tools
To find out if someone has insomnia, doctors use special screening tools. These tools check how bad someone’s sleep problems are. They look at things like how well you sleep and what affects your sleep during the day.
These questionnaires are very important. They help figure out if someone’s sleep trouble fits the official rules for insomnia. By asking the right questions, doctors can learn a lot about your sleep.
Questionnaires Used for Diagnosis
Many questionnaires are great for spotting insomnia. Some well-known ones are:
- Sleep Condition Indicator (SCI): This has eight questions and is very reliable for identifying sleep issues.
- Short-form Sleep Condition Indicator (SCI-02): It closely matches the longer SCI, making it quick for checks.
- Pittsburgh Sleep Quality Index (PSQI): This tool helps doctors understand your sleep quality over the last month.
- Insomnia Severity Index (ISI): It finds out how hard insomnia is hitting you and your day-to-day life.
The Importance of Medical History
Knowing a patient’s full medical story is key to diagnosing insomnia. It helps uncover if any past illnesses or medications might be causing sleep problems. Here’s what to keep an eye on:
- Past mental health issues, like depression or anxiety, can affect sleep.
- Long-term health conditions are also a clue to sleep troubles.
- The impact of medicines on sleep quality is crucial to know.
- How much someone worries or overthinks can make sleeping harder.
By using these screening tools and looking at medical history, doctors can accurately spot insomnia. This full view helps them make a good plan to get patients back to sleeping well. It leads to better health and happiness.
Assessing Insomnia Symptoms
Knowing how insomnia affects daily life is key. It leads to feeling tired, easily upset, and struggling to think clearly. People with insomnia have a hard time with day-to-day tasks.
Daytime Impacts of Sleep Disturbances
Insomnia’s effects reach into the day, touching all parts of life. You might see:
- Increased fatigue: You could feel too tired for work or school.
- Irritability: You might get moody, which hurts relationships.
- Cognitive impairment: Thinking or making choices can get hard.
Factors Contributing to Insomnia
Many things can cause insomnia. It’s important to know what they are to handle them well. These include:
- Lifestyle choices: Odd work hours and bad sleep habits can ruin sleep quality.
- Substance use: Drinking caffeine or alcohol can make sleeping tough.
- Psychological stress: Worry and sadness can mess with your sleep.
Understanding these factors is key for setting up plans. Such plans aim at fixing sleep issues and boosting overall health.
| Factors | Impact on Insomnia |
|---|---|
| Lifestyle Choices | Bad sleep habits lead to trouble falling and staying asleep. |
| Substance Use | Things like caffeine and alcohol mess with sleep quality. |
| Psychological Stress | Worry and stress make it hard to sleep. |
An organized plan is key to managing insomnia. It looks at all factors while checking symptoms to improve how we treat it.
Interpretation of Insomnia Diagnostic Criteria
It’s key for health workers and patients to understand insomnia’s diagnostic criteria. Knowing the difference between short-term vs. chronic insomnia is vital. It guides the diagnosis and choice of treatment. Insomnia gets classified by how long it lasts and specific symptoms. This makes the diagnosis clear.
Understanding Short-term vs. Chronic Insomnia
Short-term insomnia lasts from one to three months. It can start from stress or big life changes. Chronic insomnia lasts over three months, happening at least three nights a week. Knowing these types helps doctors find the cause of insomnia.
Specifiers for Insomnia Diagnosis
The DSM-5 added new specifiers to the insomnia disorder, making diagnosis clearer. These specifiers cover things like mental health problems and other health issues. They help understand the patient’s overall health better. Knowing if insomnia is episodic, persistent, or recurrent leads to better treatment.
Ruling out other sleep issues is also important. This makes sure insomnia isn’t due to other causes. Considering other factors like mood swings or being tired during the day is crucial. It affects how someone functions daily. This approach to diagnosis looks at various aspects. It helps choose the best management approach. For more details on diagnostic criteria, check this resource.
Conclusion
It’s important to understand the diagnostic criteria for insomnia. Doing so helps in effective treatment and management. The criteria are clear: symptoms must lead to significant distress. They should happen at least three nights a week for three months. This clarity helps healthcare professionals create effective treatments.
The rise in insomnia diagnoses shows more people need help. It’s also about better awareness. Various treatments, like Cognitive Behavioral Therapy (CBT-I), show promise. They work well for many ages.
Drugs can offer quick relief but may not work well long-term. They might also have side effects. Following the criteria helps doctors identify and help patients better. This improves life quality.
Educating people on insomnia is crucial. More awareness can lead to better management. Ongoing research is also bringing new insights. An informed society can tackle insomnia better. This could lead to better health for all.